YOUNG PROFESSIONAL CONSULTING
EMPOWER YOUR CLIENTS

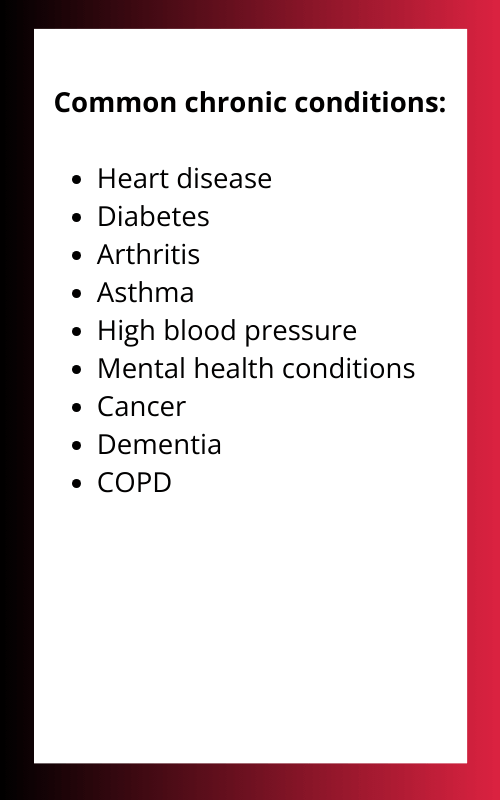
Chronic Care Management empowers healthcare organizations caring for seniors and individuals with disabilities. It helps them protect their patients, meet their comprehensive health needs, and achieve better health outcomes. This program aims to equip patients and families with a deeper understanding of their conditions, allowing them to be more prepared for most situations and live their lives as freely as possible.
what is chronic care management

HOW CLIENTS BENEFIT FROM CCM

Managing chronic conditions often faces two main hurdles: ensuring coordinated care across various providers to avoid medication conflicts and missed appointments, and addressing the social determinants of health that can worsen these conditions, such as poverty or lack of healthy food access.
As a result, these challenges can lead to poorer health outcomes, increased hospital admissions, and a lower quality of life for individuals with chronic conditions. This includes a higher risk of complications like strokes, heart attacks, and falls.
Our dedicated team of professionals, including nurses and care coordinators, works collaboratively with referring agencies, patients, families, and healthcare providers to create a personalized care plan and ensure a coordinated approach to managing chronic conditions.
Chronic Care Management Process


We look forward to our partnership in helping to improve your clients outcomes. Feel free to contact us or submit your referral so that your clients can start receiving personalized care management services.

A Little About Me
I'm a Registered Nurse and Care Management Consultant fueled by a love of technology and a passion for improving patient lives. I believe AI can revolutionize care, and I'm thrilled to partner with clients to leverage its potential. Let's work together to empower patients and build a brighter future for chronic care management!
After spending a few years as a Clinical Supervisor in an ICWP Waiver, I realized that many patients could benefit from Chronic Care Management to have better health outcomes. The rest is History!
Is there a cost for CCM services for EDWP waiver clients?
The cost of CCM services for EDWP waiver clients may vary depending on the specific program and payer requirements. It's essential to clarify the cost structure with the program provider.
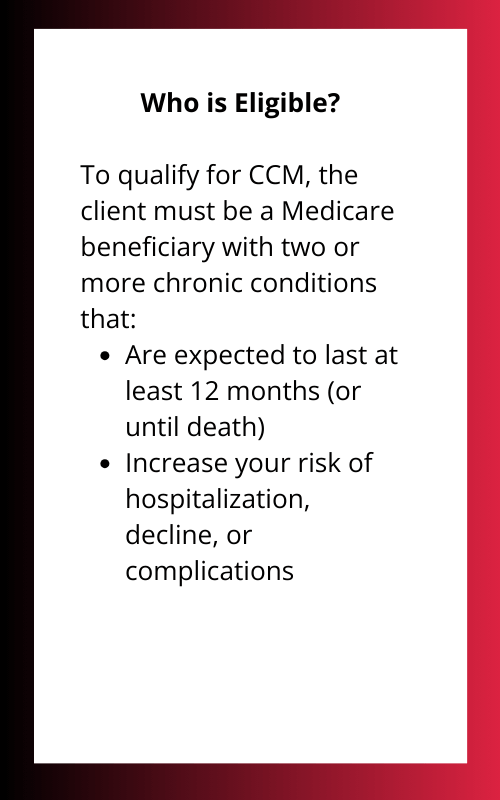
Who is eligible for CCM services?
CCM is primarily for individuals with multiple chronic conditions who require ongoing care coordination and support. Eligibility may vary based on specific program guidelines.
What services are included in CCM?
CCM services typically include care coordination, medication management, health education, and support for self-management. Specific services may vary based on the program.
How often will my clients receive CCM services?
The frequency of CCM services depends on the individual client's needs and the specific program guidelines. Typically, clients receive regular check-ins and support as needed.
How does CCM interact with existing care providers?
CCM works in collaboration with primary care physicians, specialists, and other healthcare providers to ensure coordinated and comprehensive care for the client.
How do I refer a client to the CCM program?
The referral process typically involves completing a referral form and providing relevant client information. Specific referral procedures may vary based on the program.
What is the Chronic Care Management Program (CCM)?
CCM is a program designed to support individuals with multiple chronic conditions. It provides ongoing care coordination, education, and support to help manage these conditions effectively.
What information is required for the referral?
Referral information usually includes the client's name, contact information, diagnosis, and relevant medical history.
What happens after I refer a client?
Upon receiving a referral, the CCM program will typically conduct an initial assessment to determine the client's eligibility and develop a personalized care plan.



